When you understand your eye conditions, there's collaboration in care
At Advanced Eye Care of Tucson, we strive and pride ourselves in excellent communication with and educating patients on their diagnosis and treatment plan. Please read through our resources for details and information.

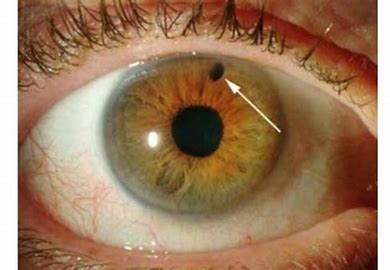
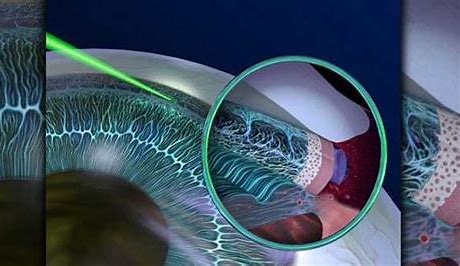
Narrow Angles & Laser Peripheral Iridotomy
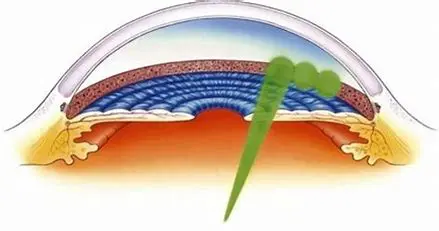
“Narrow angles” is a term that describes the shape of the drainage angle of the eye, where fluid called aqueous humor drains from the eye, When the iris and the cornea are too close together, they can block the fluid from leaving the eye, causing a sudden and dangerous increase in eye pressure. This condition is called narrow angle glaucoma and is a medical eye emergency.
Narrow angles often is a precursor to angle-closure glaucoma, the kind of glaucoma that can have a sudden, painful onset leading to permanent vision loss.
The best time to prevent the damage that angle-closure glaucoma can cause is to treat it with a laser iridotomy before the actual disease sets in. This is a vision saving procedure at its best.
Although not everyone with narrow angles actually develops glaucoma, careful evaluation of the angle structure can identify who is at greatest risk. The angle structure is determined by an examination called gonioscopy. Dr. Tsai then expertly evaluates the degree of risk and makes his professional recommendation.
By performing a laser iridotomy, Dr. Tsai is trying to save you from the risk of acute angle-closure glaucoma.
Keep in mind potential Laser Peripheral Iridotomy side effects:
The theory is that the tear film at the edge of the eyelid creates a prism that bends the light and allows it to get underneath the lid and through the PI, finally hitting the retina. The nature of the refractory path creates a focused image on the retina, causing “line in vision” post LPI.
Creating a hole through the iris can invite optical aberration, and many patients experience dysphotopsias following the procedure.
Fortunately, if a dysphotopsia does occur postop, it often resolves over time.
Remember that Dr. Tsai performs an LPI to prevent glaucomatous visual loss, prevent ACUTE ANGLE CLOSURE ATTACK, treat anatomical narrow angles.
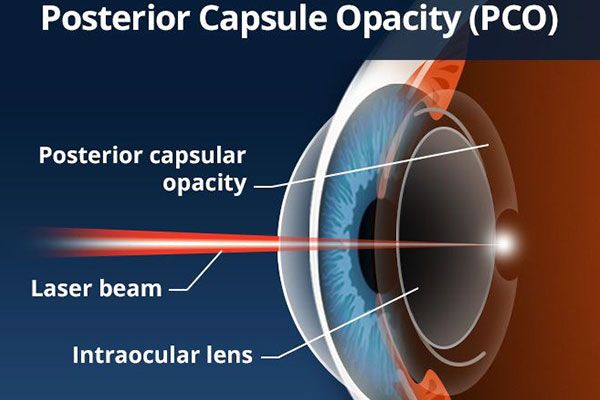
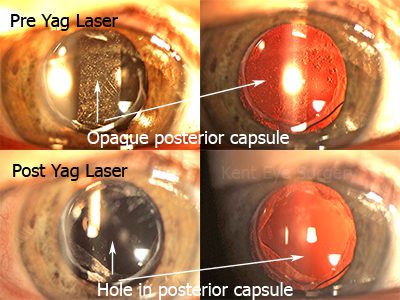
Posterior Capsular Opacification and YAG Laser Treatment
Posterior capsulotomy (or YAG laser capsulotomy) is laser surgery you might need sometime after cataract surgery. It helps you see clearly if your vision becomes cloudy again.
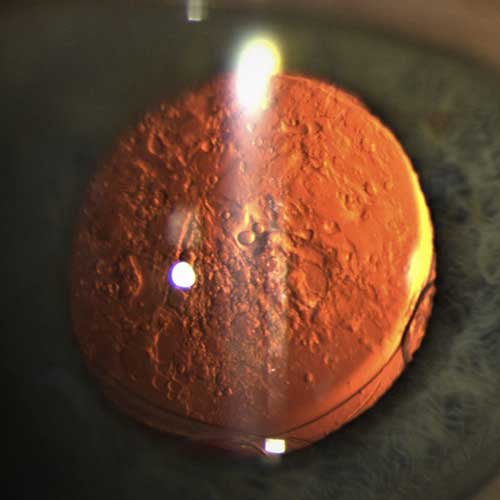
When you have cataract surgery, your ophthalmologist removes your eye's cloudy lens. They replace it with a clear, artificial intraocular lens (IOL). The IOL is held in place in the eye’s natural lens capsule. Weeks, months or years later, this capsule can become cloudy or wrinkled, causing blurry vision. This is called a posterior capsule opacification (PCO). It’s also sometimes called a "secondary cataract" or "scar tissue." With posterior capsulotomy, a laser is used to make an opening in the cloudy capsule. This allows light to pass through again for clear vision.
What Happens During Posterior Capsulotomy?
The procedure is done in your ophthalmologist's office or an outpatient surgery center. It only takes about 5 minutes. Here is what will happen:
- Your eye will be numbed with eye drops. You may be given other eye drops as well to dilate your pupil.
- Your ophthalmologist will point a special laser at the back of the lens capsule and make a small opening.
- Once your vision is clear after the procedure, you can usually do all of your normal daily activities. But you may need to have someone drive you home. Your ophthalmologist will tell you if there are things you should not do right after surgery.
- You may need to use eye-drop medicine for a few days after the surgery. Your ophthalmologist will let you know if this is necessary.
- If you have no other eye problems affecting your vision, your sight should improve in about 24 hours.
What Are the Risks of Posterior Capsulotomy?
As with any surgery, there are possible risks and complications with posterior capsulotomy. Here are some of them:
- You may have a detached retina (where the tissue lifts from the back of your eye). You may see what looks like a gray curtain moving across your field of vision. You might also see a lot of floaters or flashes of light. You should call your ophthalmologist immediately if this happens to your vision.
- The pressure in your eye may increase.
- The IOL might move through the posterior capsule opening.
- You may have swelling in your eye, and you may need steroid eye drops.
SELECTIVE LASER TRABECULOPLASTY (SLT)
A LASER PROCEDURE TO POTENTIALLY LOWER EYE PRESSURE
What is SLT?
SLT is a laser procedure performed in the office to lower eye pressure.
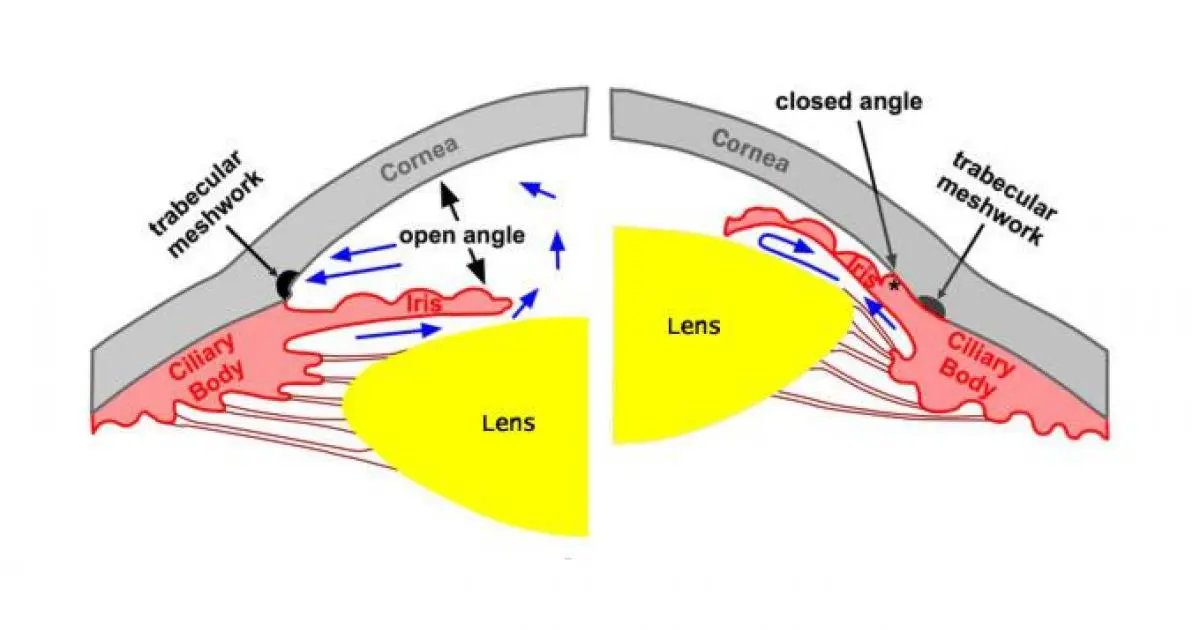
How does SLT work?
Laser energy is applied to the trabecular meshwork. The trabecular meshwork is located in the front of the eye and is the natural drain for fluid. SLT stimulates the trabecular meshwork to increase the amount of fluid drained from within the eye, which lowers eye pressure. It may take up to 2 months for the laser to take its full effect.
Who needs SLT?
Patients with open-angle glaucoma who need improvement in eye pressure control. This can be used alone or as an addition to eye drops.
What are the benefits?
On average, SLT can lower the eye pressure by about 20-30%. The laser is effective in lowering eye pressure in about 80% of patients. The laser effect wears off after several years, but the trabecular meshwork can be stimulated again with repeat laser. SLT does not affect the success rates or the eligibility of getting other medical or surgical treatments.
What are the risks?
Compared to many other treatments for glaucoma, including eye drops, other laser treatments and surgery, SLT has few side effects. Inflammation is possible after the laser but it is not common. You may be prescribed anti-inflammatory drops on an individual basis. There is a small risk of temporary high eye pressures shortly following the laser treatment. This is usually controlled with glaucoma medications.
Will SLT cure my glaucoma?
The simple answer is “No”. Glaucoma is a chronic disease that requires constant monitoring and treatment. The SLT procedure will help to lower your eye pressure. However, it will not reverse any loss of vision that has already occurred.

What should I expect if I have an SLT?
Your treatment will be performed in a specially equipped laser room in the clinic. Once you have been checked in, drops will be used to numb your eye and check the pressure. No injections or needles will be used.
- First, you will receive an eye drop which helps prevent a rise in the eye pressure after the procedure. Then a drop of anesthetic will be applied to numb the eye.
- Tsai will place a special lens on your eye to help focus the laser on the trabecular meshwork. This lens also prevents your eye from blinking and keeps the eye still during the treatment. A clear gel is placed between the eye and the lens to protect the surface of your eye.
- You will then hear a series of clicks and may see flashes of light as the laser treats your eye. There is virtually no pain with the procedure. You will feel the lens slowly rotating on the surface of the eye as Dr. Tsai treats various parts of the trabecular meshwork. The procedure generally takes a few minutes.
What should I expect after SLT?
At the end of the laser treatment, the lens will be removed from the eye. The gel may remain on your eye for up to an hour, leading to blurred vision or a feeling of heaviness. As a safety measure, your eye pressure will be checked sometime after your procedure.
How long after the laser I will be seen?
We do two post procedure visits: approximately 2 weeks after laser and 6 weeks after the laser.
What eye drops will I use after the laser procedure?
Dr. Tsai may ask you to use an anti-inflammatory eye drop in the treated eye for several days.
Can I stop my glaucoma drops after the laser procedure?
Dr. Tsai will tell you which drops to continue using and how often after the laser procedure. Sometimes patients are able to reduce the number of eye drops they are taking. Even if you are taking the same glaucoma medications after the procedure, the surgery is a success if your pressure is lower. The need for eye drops long-term after this treatment varies greatly and depends on your type of glaucoma and the rate at which it is progressing.
Will my vision improve after the laser procedure?
This laser is for lowering the eye pressure and will not improve or affect your vision.
What is the recovery time and what should I expect?
- Though everyone heals differently, most people can resume normal activities right after treatment, although you'll need to have someone drive you home. For the next few days your eyes may be red, a little scratchy and sensitive to light if you develop inflammation in the eye after the procedure
- If there is any blurred vision, it usually improves within hours or a day or so.
- There are no restrictions in reading, watching TV, using your phone, tablet device, computer, etc but you may tire more easily during these activities.
- Tylenol (acetaminophen) or ibuprofen is a good option if you feel any pain or discomfort unless you are unable to take these medication.
- If your eye has severe pain or sudden worsening pain or vision after surgery, please call our office immediately.
Will SLT cure my glaucoma?
The simple answer is “No”. Glaucoma is a chronic disease that requires constant monitoring and treatment. The SLT procedure will help to lower your eye pressure. However, it will not reverse any loss of vision that has already occurred.